Guaranteed Savings
0% Payments
Nationwide Access
ClaimsAssist Plus™ — Voluntary Member Savings
Instant savings and flexible 0% payments — for every employee, everywhere.
ClaimsAssist Plus™ lowers medical costs automatically and makes every bill easier to manage. Members see savings applied right away, can pay over time at 0% interest, and receive proactive checks for additional assistance—without changing their health plan. Offered through employers as a voluntary, employee-paid benefit.
The Employer Challenge
- Rising out-of-pocket costs create financial stress and impact retention.
- Confusing bills drive HR escalations and lower satisfaction.
- Unpredictable savings make budgeting difficult for employers and members.
The Solution & Savings
Built-In Provider Savings
Preferential rates at partner health systems are applied automatically—no employee action required.
Advocacy + Bill Clarity
Our advocates review bills, negotiate savings, and guide employees to resolution.
Simple, Flexible Payments
Pay in full for the highest discount or choose 0% interest installments.
- Up to 13% off automatically at participating regional health systems.
- 0% interest payment options reduce employee stress and HR escalations.
- Financial-assistance savings typically 25–60% for eligible members; group-wide averages ~10–25%.
Discounts and 0% options vary by provider and eligibility.
Lower member out-of-pocket
Predictable employer savings
Stronger broker differentiation
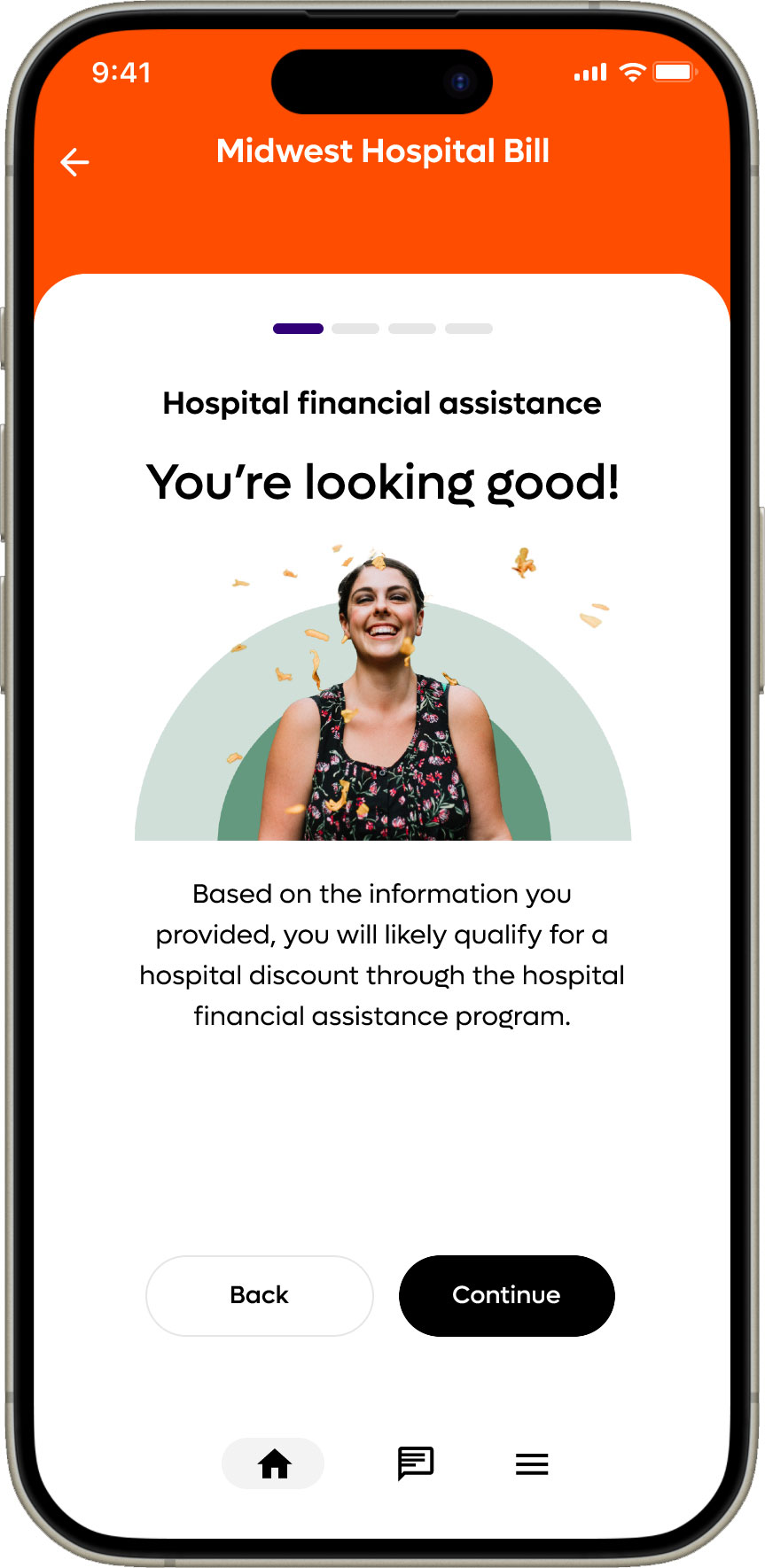
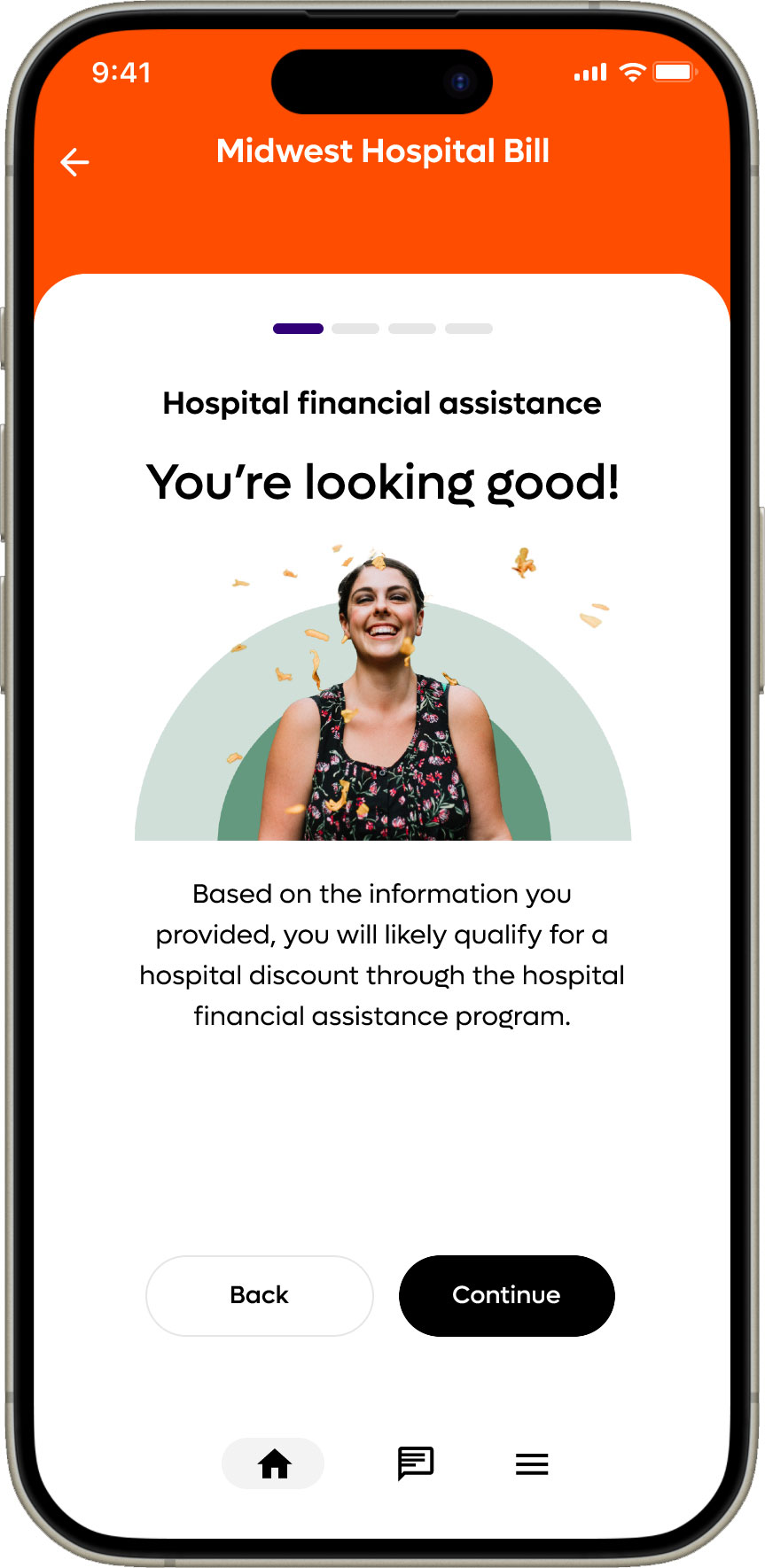
How It Works (in the app)
- 📞Search high-value providers to compare options and estimated savings.
- ⏱️See real-time savings + 0% payments for each bill.
- 💻Track bills and advocacy updates with push/email alerts.
How Savings Are Applied (At or After Care)
1
Claim or Visit Detected
Member presents BeneBridge ID at a participating provider or a claim is received automatically from the health system or TPA.
2
Savings Verified & Applied
Partner rates or financial-assistance savings are checked, validated, and applied automatically.
3
Member Chooses Payment
Pay in full to maximize the discount or select 0% interest installments.
Go Further
Optional Enhancements
AdvocateAssist™: White-glove help on complex bills. Experts review coding, dispute errors, and negotiate charges—members can opt in per claim. Pay-for-performance: members pay only a share of verified negotiated savings (no PEPM).
Optional Claim Feed Integration: Employers may authorize MediBridge to receive claim notifications from their TPA for proactive outreach and guidance. Not required for the voluntary program.